Disclaimer
The alfapump® system is currently not approved in Canada for commercial use. DSR® therapy is still in development and is currently not approved in the United States or Canada. Any statements regarding safety and efficacy arise from ongoing pre-clinical and clinical investigations which have yet to be completed. Sequana Medical makes no claims of safety or effectiveness of the DSR® therapy in the U.S. or Canada. There is no link between the DSR® therapy and ongoing investigations with the alfapump® system in Europe, the United States or Canada.
Cirrhosis is late-stage liver disease which occurs when scar tissue (fibrosis) replaces healthy tissue. Alcohol and viral hepatitis B and C are common causes of cirrhosis, although there are many other causes including Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) and Metabolic Dysfunction-Associated Steatohepatitis (MASH).
The incidence of liver disease and liver cirrhosis is increasing driven by unhealthy lifestyles, obesity and ageing populations.
Chronic liver disease and cirrhosis are one of the fastest growing leading causes of death in the U.S [source]
MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) (formerly NAFLD) and MASH (Metabolic Dysfunction-Associated Steatohepatitis) (formerly NASH) are both closely associated with diabetes and obesity.
The U.S. prevalence of MASH is expected to increase by 63% from 2015 to 2030. [source]
MASLD is fatty infiltrations in the liver not caused by alcohol which can then lead to MASH, a more serious stage of the disease where the liver becomes inflamed due to the accumulation of fat. It is estimated there will be between three and four million people in the U.S. suffering from liver cirrhosis due to MASH in the near to medium term based on the current prevalence of MASH in the U.S. population and the observed rates at which MASH patients develop cirrhosis [source].
MASH is a “silent disease”, which means it is difficult to diagnose until the disease is significantly developed and therefore intervention at an early stage to prevent the fibrosis and scarring is clinically challenging.
Ascites, the accumulation of fluid in the abdomen, is a key complication of liver cirrhosis. Approximately 50% of cirrhotic patients develop ascites within ten years of the diagnosis of cirrhosis. [source]
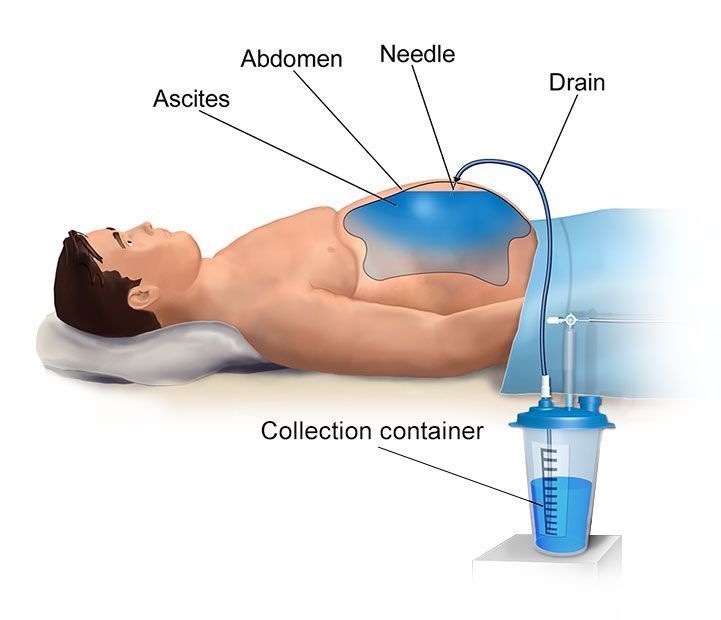
Management of ascites is primarily based on a low-sodium diet and diuretic treatment. When drug therapy and dietary restriction are no longer effective, the common treatment is paracentesis, an invasive procedure in which a large-bore needle is inserted into the abdomen, to drain the fluid over a period of a few hours. Paracentesis of more than 5 liters is referred to as large volume paracentesis (LVP).
Approximately 7.5% of patients with cirrhosis and ascites will develop liver refractory ascites, which is ascites that is unresponsive to a sodium-restricted diet and high-dose diuretic treatment or that recurs rapidly after paracentesis. [source]
Recurrent ascites is a severe stage prior to further progression to refractory ascites and is defined as ascites that recurs on at least 3 occasions within a 12-month period despite prescription of dietary sodium restriction and adequate diuretic dosage.
Ascites has a dramatic negative impact on patient quality of life including difficulties in eating, moving, breathing and sleeping. Patients with ascites suffer from malnutrition, withdrawal from society, nausea, serious infection risks, swelling and tension.
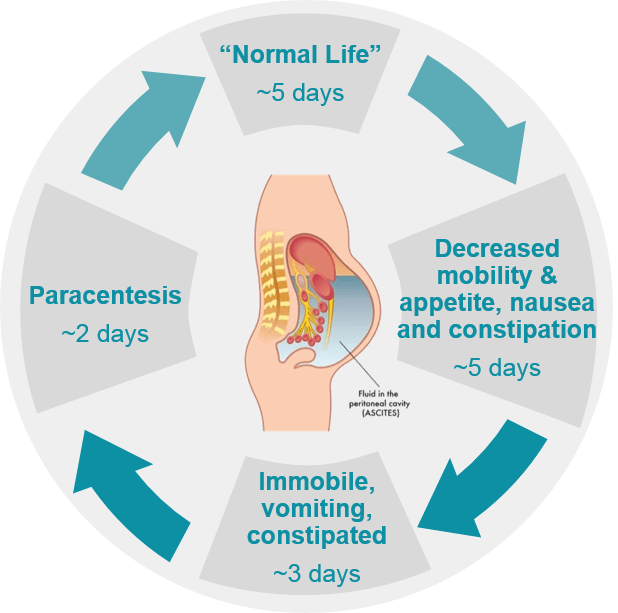
Typical life for a patient with refractory ascites
Patients may accumulate as much as 10-15 lites of ascites every 15 days. When large quantities of ascites accumulate in the abdominal cavity, the sheer volume of liquid puts pressure on the surrounding organs such as the bladder, stomach and even diaphragm. In addition to making it difficult to move around, common symptoms include fatigue, shortness of breath and some pain. Pressure on the stomach can lead to loss of appetite and heartburn, ultimately resulting in malnutrition, and constant shortness of breath can limit a patient’s capacity to perform even minor everyday tasks. Too much pressure inside the abdomen can lead to the development of hernias around the belly button or in the groin. Patients with ascites are also at high risk of other complications, such as severe internal infections and kidney problems.
Until the alfapump®, treatment options for refractory ascites have been limited and unsatisfactory for some patients, leaving both patients and doctors in need of a better solution.
The standard of care for refractory ascites is LVP with albumin infusion to decrease the risk of paracentesis-induced circulatory dysfunction. Although LVP is generally considered safe, it is a painful and burdensome procedure which only provides short-term symptomatic relief as it needs to be repeated when the ascites re-accumulates.
In the meantime the patient is left feeling bloated and unwell as the fluid continues to collect, which together with the regular visit to the hospital severely impacts the patients’ quality of life. The repeated procedures are also a significant cost and burden on the patient and healthcare systems.
In some patients with liver refractory ascites, a therapeutic alternative to repeated LVPs is the use of a transjugular intrahepatic portosystemic shunt (TIPS). A TIPS is a shunt to re-route a significant proportion of the blood flow around the damaged liver into the main blood vessels. The reduction in blood flow through the liver results in less filtering out of toxic substances in the blood stream and results in an increased risk of hepatic encephalopathy, which develops in 30-50% of the patients, and which further increases with age [source].
As a result, TIPS carries significant risks for patients over 65 years old, —a demographic that includes many individuals expected to develop ascites due to MASH.
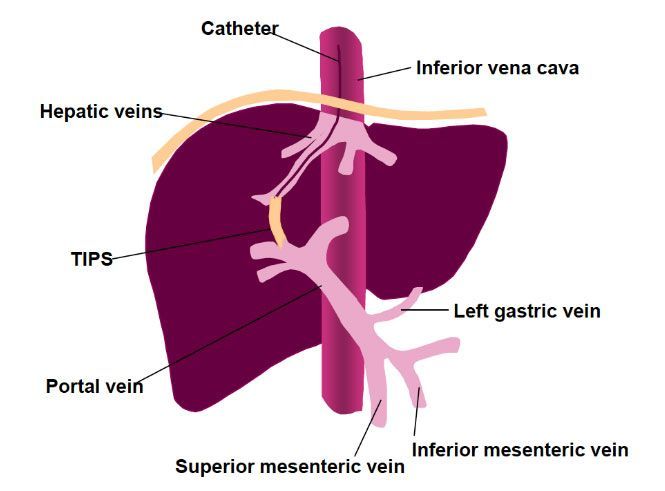
Transjugular Intrahepatic Portosystemic Shunt (TIPS)
The only cure for liver disease is a liver transplant. Liver transplants are very limited in availability and result in large healthcare costs. Lifelong use of immunosuppression drugs is required to reduce the risk that the recipient’s body will reject the transplant.
Liver transplant